Fitness
Effects of different types of exercise intensity on improving health-related physical fitness in children and adolescents: a systematic review – Scientific Reports
Jebeile, H., Kelly, A. S., O’Malley, G. & Baur, L. A. Obesity in children and adolescents: epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 10, 351–365. https://doi.org/10.1016/s2213-8587(22)00047-x (2022).
Ezzati, M. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3 (2017).
Simmonds, M., Llewellyn, A., Owen, C. G. & Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obesity Rev. 17, 95–107. https://doi.org/10.1111/obr.12334 (2016).
The, N. S., Suchindran, C., North, K. E., Popkin, B. M. & Gordon-Larsen, P. Association of adolescent obesity with risk of severe obesity in adulthood. Jama-J. Am. Med. Associat. 304, 2042–2047. https://doi.org/10.1001/jama.2010.1635 (2010).
Horesh, A., Tsur, A. M., Bardugo, A. & Twig, G. Adolescent and childhood obesity and excess morbidity and mortality in young adulthood-a systematic review. Curr. Obesity Rep. 10, 301–310. https://doi.org/10.1007/s13679-021-00439-9 (2021).
Jebeile, H., Cardel, M. I., Kyle, T. K. & Jastreboff, A. M. Addressing psychosocial health in the treatment and care of adolescents with obesity. Obesity 29, 1413–1422. https://doi.org/10.1002/oby.23194 (2021).
Weihrauch-Blueher, S., Schwarz, P. & Klusmann, J.-H. Childhood obesity: Increased risk for cardiometabolic disease and cancer in adulthood. Metabolism-Clin. Exp. 92, 147–152. https://doi.org/10.1016/j.metabol.2018.12.001 (2019).
Li, J., Zhou, X., Huang, Z. & Shao, T. Effect of exercise intervention on depression in children and adolescents: a systematic review and network meta-analysis. Bmc Public Health https://doi.org/10.1186/s12889-023-16824-z (2023).
Romero-Perez, E. M. et al. Influence of a physical exercise program in the anxiety and depression in children with obesity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17134655 (2020).
Martin, A. et al. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Systematic Rev. https://doi.org/10.1002/14651858.CD009728.pub3 (2018).
Cai, Y., Zhu, X. & Wu, X. Overweight, obesity, and screen-time viewing among Chinese school-aged children: National prevalence estimates from the 2016 Physical Activity and Fitness in China-The Youth Study. J. Sport Health Sci. 6, 404–409. https://doi.org/10.1016/j.jshs.2017.09.002 (2017).
Sedgwick, M. J., Morris, J. G., Nevill, M. E. & Barrett, L. A. Effect of repeated sprints on postprandial endothelial function and triacylglycerol concentrations in adolescent boys. J. Sports Sci. 33, 806–816. https://doi.org/10.1080/02640414.2014.964749 (2015).
Costigan, S. A., Eather, N., Plotnikoff, R. C., Taaffe, D. R. & Lubans, D. R. High-intensity interval training for improving health-related fitness in adolescents: A systematic review and meta-analysis. Br. J. Sports Med. https://doi.org/10.1136/bjsports-2014-094490 (2015).
Donnelly, J. E. et al. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exercise 41, 459–471. https://doi.org/10.1249/MSS.0b013e3181949333 (2009).
Reilly, J. J. & Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obesity 35, 891–898. https://doi.org/10.1038/ijo.2010.222 (2011).
Hopkins, N. D. et al. Relationships between measures of fitness, physical activity, body composition and vascular function in children. Atherosclerosis 204, 244–249. https://doi.org/10.1016/j.atherosclerosis.2008.09.004 (2009).
Chuensiri, N., Suksom, D. & Tanaka, H. Effects of high-intensity intermittent training on vascular function in obese preadolescent boys. Childhood Obesity 14, 41–49. https://doi.org/10.1089/chi.2017.002 (2018).
Weston, K. S., Wisloff, U. & Coombes, J. S. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: A systematic review and meta-analysis. Br. J. Sports Med. 48, 1227-U1252. https://doi.org/10.1136/bjsports-2013-092576 (2014).
Corbin, C. B., Welk, G. J., Corbin, W. R. & Welk, K. A. Concepts of Physical Fitness: Active Lifestyles for Wellness 14th edn. (William Glass, 2008).
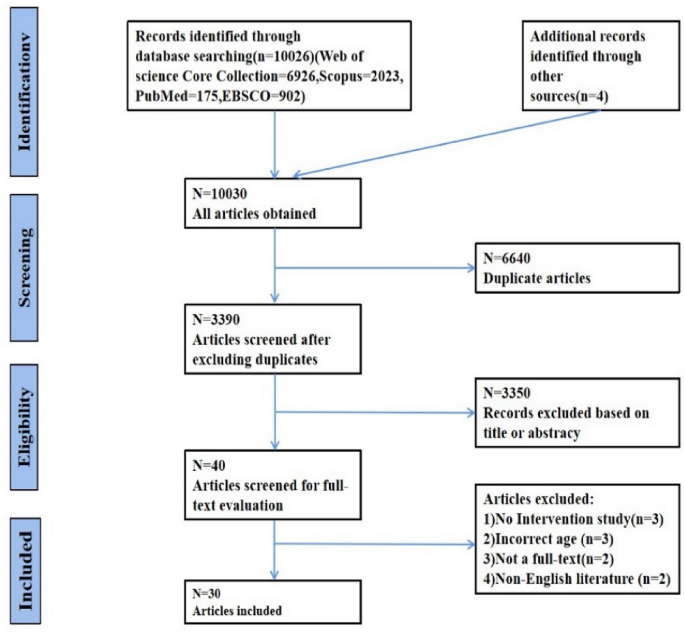
Hutton, B., Caldwell, D. M., Chaimani, A., Schmid, C. H. & Cameron, C. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Internal Med. 162(11), 777–784. https://doi.org/10.7326/M14-2385 (2015).
Vrabel, M. Preferred reporting items for systematic reviews and meta-analyses. Oncol. Nursing Forum 42, 552–554. https://doi.org/10.1188/15.Onf.552-554 (2015).
Adolescent health in the South-East Asia Region, https://www.who.int/southeastasia/health-topics/adolescent-health> (2022).
de Morton, N. A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 55, 129–133. https://doi.org/10.1016/s0004-9514(09)70043-1 (2009).
Farah, B. Q., Ritti-Dias, R. M., Balagopal, P., Hill, J. O. & Prado, W. L. Does exercise intensity affect blood pressure and heart rate in obese adolescents? A 6-month multidisciplinary randomized intervention study. Pediatric Obesity 9, 111–120. https://doi.org/10.1111/j.2047-6310.2012.00145.x (2014).
Hay, J. et al. Physical activity intensity and type 2 diabetes risk in overweight youth: a randomized trial. Int. J. Obesity 40, 607–614. https://doi.org/10.1038/ijo.2015.241 (2016).
Bond, B. et al. Exercise intensity and the protection from postprandial vascular dysfunction in adolescents. Am. J. Physiol. -Heart Circulatory Physiol. 308, H1443–H1450. https://doi.org/10.1152/ajpheart.00074.2015 (2015).
Paravidino, V. B., Felix Mediano, M. F., Hoffman, D. J. & Sichieri, R. Effect of exercise intensity on spontaneous physical activity energy expenditure in overweight boys: A crossover study. Plos One https://doi.org/10.1371/journal.pone.0147141 (2016).
Tadiotto, M. C. et al. Effects and individual response of continuous and interval training on adiponectin concentration, cardiometabolic risk factors, and physical fitness in overweight adolescents. Eur. J. Pediatr. 182, 2881–2889. https://doi.org/10.1007/s00431-023-04974-6 (2023).
Larsen, M. N. et al. Positive effects on bone mineralisation and muscular fitness after 10 months of intense school-based physical training for children aged 8–10 years: The FIT FIRST randomised controlled trial. Br. J. Sports Med. 52, 254. https://doi.org/10.1136/bjsports-2016-096219 (2018).
Ramirez-Velez, R. et al. Effects of different doses of exercise on inflammation markers among adolescents with overweight/obesity: HEPAFIT study. J. Clin. Endocrinol. Metabolism 107, E2619–E2627. https://doi.org/10.1210/clinem/dgac021 (2022).
Cao, M., Tang, Y., Li, S. & Zou, Y. Effects of school-based high-intensity interval training on body composition, cardiorespiratory fitness and cardiometabolic markers in adolescent boys with obesity: A randomized controlled trial. Bmc Pediatr. https://doi.org/10.1186/s12887-021-03079-z (2022).
Dias, K. A. et al. Effect of high-intensity interval training on fitness, fat mass and cardiometabolic biomarkers in children with obesity: A randomised controlled trial. Sports Med. 48, 733–746. https://doi.org/10.1007/s40279-017-0777-0 (2018).
Faigenbaum, A. D., Westcott, W. L., Loud, R. L. & Long, C. The effects of different resistance training protocols on muscular strength and endurance development in children. Pediatrics 104, e5–e5. https://doi.org/10.1542/peds.104.1.e5 (1999).
Benson, A. C., Torode, M. E. & Singh, M. A. F. The effect of high-intensity progressive resistance training on adiposity in children: A randomized controlled trial. Int. J. Obesity 32, 1016–1027. https://doi.org/10.1038/ijo.2008.5 (2008).
Taber, D. R. et al. Participation in vigorous sports, not moderate sports, is positively associated with cardiorespiratory fitness among adolescent girls. J. Phys. Activity Health 11, 596–603. https://doi.org/10.1123/jpah.2011-0280 (2014).
Davis, C. L. et al. Exercise dose and diabetes risk in overweight and obese children a randomized controlled trial. Jama-J. Am. Med. Associat. 308, 1103–1112. https://doi.org/10.1001/2012.jama.10762 (2012).
Burns, S. F., Oo, H. H. & Anh Thanh Thuy, T. Effect of sprint interval exercise on postexercise metabolism and blood pressure in adolescents. Int. J. Sport Nutr. Exerc. Metabolism 22, 47–54. https://doi.org/10.1123/ijsnem.22.1.47 (2012).
Leppanen, M. H. et al. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: Results from the ministop trial. Int. J. Obesity 40, 1126–1133. https://doi.org/10.1038/ijo.2016.54 (2016).
Leppanen, M. H. et al. Longitudinal physical activity, body composition, and physical fitness in preschoolers. Med. Sci. Sports Exerc. 49, 2078–2085. https://doi.org/10.1249/mss.0000000000001313 (2017).
Gomes, P. P., Silva, H. J. G. D., Lira, C. T. C. D., Lofrano-Prado, M. C. & Prado, W. L. D. Efeitos de diferentes intensidades de treinamento aeróbio sobre a composição corporal em adolescentes obesos. Revista Brasileira de Cineantropometria Desempenho Humano 15, 594–603. https://doi.org/10.5007/1980-0037.2013v15n5p594 (2013).
Buchan, D. S. et al. High intensity interval running enhances measures of physical fitness but not metabolic measures of cardiovascular disease risk in healthy adolescents. BMC Public Health 13, 498–498. https://doi.org/10.1186/1471-2458-13-498 (2013).
Grasten, A., Huhtiniemi, M., Kolunsarka, I. & Jaakkola, T. Developmental associations of accelerometer measured moderate-to-vigorous physical activity and sedentary time with cardiorespiratory fitness in schoolchildren. J. Sci. Med. Sport 25, 884–889. https://doi.org/10.1016/j.jsams.2022.08.015 (2022).
Costigan, S. A. et al. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: A pilot randomized controlled trial. Prevent. Med. Rep. 2, 973–979. https://doi.org/10.1016/j.pmedr.2015.11.001 (2015).
Saidi, O. et al. Acute effect of an intensified exercise program on subsequent sleep, dietary intake, and performance in junior rugby players. Eur. J. Appl. Physiol. 119, 2075–2082. https://doi.org/10.1007/s00421-019-04196-5 (2019).
Saidi, O., Rochette, E., Bovet, M., Merlin, E. & Duche, P. Acute intense exercise improves sleep and decreases next morning consumption of energy-dense food in adolescent girls with obesity and evening chronotype. Pediatric Obesity https://doi.org/10.1111/ijpo.12613 (2020).
Gerber, M. et al. Moderate-to-vigorous physical activity is associated with cardiorespiratory fitness among primary schoolchildren living in cote D’ivoire, South Africa, and Tanzania. Front. Public Health https://doi.org/10.3389/fpubh.2021.671782 (2021).
Winn, C. O. N. et al. Effect of high-intensity interval training in adolescents with asthma: The exercise for asthma with Commando Joe’s (R) (X4ACJ) trial. J. Sport Health Sci. 10, 488–498. https://doi.org/10.1016/j.jshs.2019.05.009 (2021).
da Silva, P., Bento, A. F., Paez, L. C., de Mendonca, M. & Raimundo, A. High-intensity interval training in high-school physical education classes: Study protocol for a randomized controlled trial. Contemporary Clin. Trials Commun. 24, 100867–100867. https://doi.org/10.1016/j.conctc.2021.100867 (2021).
Videira-Silva, A., Sardinha, L. B. B. & Fonseca, H. Atherosclerosis prevention in adolescents with obesity: The role of moderate-vigorous physical activity. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph192315537 (2022).
Juric, P., Dudley, D. A. & Petocz, P. Does incorporating high intensity interval training in physical education classes improve fitness outcomes of students? A cluster randomized controlled trial. Prevent. Med. Rep. 32, 102127–102127. https://doi.org/10.1016/j.pmedr.2023.102127 (2023).
Farpour-Lambert, N. J. et al. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J. Am. College Cardiol. 54, 2396–2406. https://doi.org/10.1016/j.jacc.2009.08.030 (2009).
Ketelhut, S., Ketelhut, K., Ketelhut, S. R. & Ketelhut, R. G. Effects of school-based high-intensity interval training on hemodynamic parameters and heart rate variability: A randomized controlled trial. J. Strength Cond. Res. https://doi.org/10.1519/jsc.0000000000004744 (2024).
Migueles, J. H. et al. Effects of an exercise program on cardiometabolic and mental health in children with overweight or obesity a secondary analysis of a randomized clinical trial. Jama Netw. Open https://doi.org/10.1001/jamanetworkopen.2023.24839 (2023).
Batacan, R. B. Jr., Duncan, M. J., Dalbo, V. J., Tucker, P. S. & Fenning, A. S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. https://doi.org/10.1136/bjsports-2015-095841 (2017).
Hao, Z. et al. Which exercise interventions are more helpful in treating primary obesity in young adults? A systematic review and Bayesian network meta-analysis. Archiv. Med. Sci. 19, 865–883. https://doi.org/10.5114/aoms/153479 (2023).
Borsheim, E. & Bahr, R. Effect of exercise intensity, duration and mode on post-exercise oxygen consumption. Sports medicine (Auckland, NZ) 33, 1037–1060 (2003).
Sindorf, M. A. G. et al. Excess post-exercise oxygen consumption and substrate oxidation following high-intensity interval training: Effects of recovery manipulation. Int. J. Exerc. Sci. 14, 1151–1165 (2021).
Kargarfard, M. et al. Effects of endurance and high intensity training on ICAM-1 and VCAM-1 levels and arterial pressure in obese and normal weight adolescents. Physician Sportsmedicine 44, 208–216. https://doi.org/10.1080/00913847.2016.1200442 (2016).
Buchan, D. S. et al. The effects of time and intensity of exercise on novel and established markers of CVD in adolescent youth. Am. J. Hum. Biol. 23, 517–526. https://doi.org/10.1002/ajhb.21166 (2011).
Martin-Smith, R. et al. High intensity interval training (HIIT) improves cardiorespiratory fitness (CRF) in healthy, overweight and obese adolescents: A systematic review and meta-analysis of controlled studies. Int. J. Environ. Res. Public Health 17(8), 2955. https://doi.org/10.3390/ijerph17082955 (2020).
Cao, M., Tang, Y., Li, S. & Zou, Y. Effects of high-intensity interval training and moderate-intensity continuous training on cardiometabolic risk factors in overweight and obesity children and adolescents: A meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph182211905 (2021).
Bond, B., Weston, K. L., Williams, C. A. & Barker, A. R. Perspectives on high-intensity interval exercise for health promotion in children and adolescents. Open Access J. Sports Med. 8, 243–265. https://doi.org/10.2147/oajsm.S127395 (2017).
Little, J. P. et al. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. J. Appl. Physiol. 111, 1554–1560. https://doi.org/10.1152/japplphysiol.00921.2011 (2011).
Gibala, M. J. et al. Brief intense interval exercise activates AMPK and p38 MAPK signaling and increases the expression of PGC-1α in human skeletal muscle. J. Appl. Physiol. 106, 929–934. https://doi.org/10.1152/japplphysiol.90880.2008 (2009).
Little, J. P., Safdar, A., Bishop, D., Tarnopolsky, M. A. & Gibala, M. J. An acute bout of high-intensity interval training increases the nuclear abundance of PGC-1α and activates mitochondrial biogenesis in human skeletal muscle. Am. J. Physiol. -Regulatory Integrative Comparative Physiol. 300, R1303–R1310. https://doi.org/10.1152/ajpregu.00538.2010 (2011).
Wearing, S. C., Hennig, E. M., Byrne, N. M., Steele, J. R. & Hills, A. P. The impact of childhood obesity on musculoskeletal form. Obesity Rev.: Off. J. Int. Associat. Study Obesity 7, 209–218. https://doi.org/10.1111/j.1467-789X.2006.00216.x (2006).
Janssen, I. & LeBlanc, A. G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Activity https://doi.org/10.1186/1479-5868-7-40 (2010).
Smith, J. J. et al. Behavioral correlates of muscular fitness in children and adolescents: A systematic review. Sports Med. 49, 887–904. https://doi.org/10.1007/s40279-019-01089-7 (2019).
Holland, G. J., Tanaka, K., Shigematsu, R. & Nakagaichi, M. Flexibility and physical functions of older adults: A review. Aging Phys. Activity https://doi.org/10.1123/japa.10.2.169 (2002).
Badley, E. M., Wagstaff, S. & Wood, P. H. Measures of functional ability (disability) in arthritis in relation to impairment of range of joint movement. Ann. Rheumatic Diseases 43, 563–569. https://doi.org/10.1136/ard.43.4.563 (1984).
D’Onofrio, G., Kirschner, J., Prather, H., Goldman, D. & Rozanski, A. Musculoskeletal exercise: Its role in promoting health and longevity. Progr. Cardiovasc. Diseases 77, 25–36. https://doi.org/10.1016/j.pcad.2023.02.006 (2023).
Cvetkovic, N. et al. Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scandinavian J. Med. Sci. Sports 28, 18–32. https://doi.org/10.1111/sms.13241 (2018).
Liu, C., Cao, Y., Zhang, Z., Gao, R. & Qu, G. Correlation of fundamental movement skills with health-related fitness elements in children and adolescents: A systematic review. Front. Public Health https://doi.org/10.3389/fpubh.2023.1129258 (2023).








