Fitness
Examining the mediating role of muscle quantity in adolescents: associations with adiposity, cardiorespiratory fitness, muscular fitness, and cardiometabolic risk factors – Scientific Reports
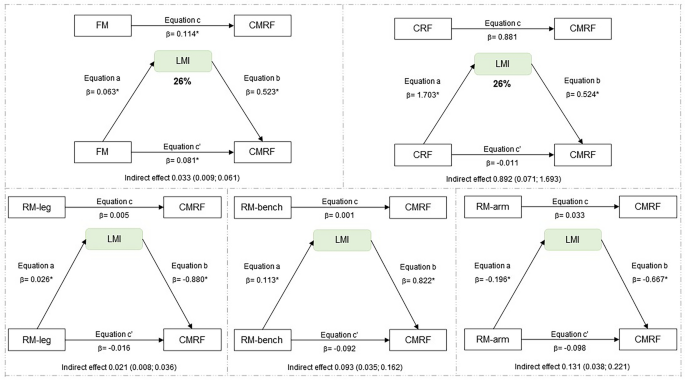
In this study, the main findings indicate that muscle quantity shows a 26% mediation between CRF and CMRF in the total sample, whose relationship is most evident for girls (32%). LMI mediates 32% between fat mass and CRMF. Regarding MFR, a 16% mediation effect was observed between RM-leg press and CMRF, being found as 25% in boys and 22% in girls. However, the other indicators of muscle quantity assessed by the appendicular skeletal results, both ASM and ASMI showed no mediating effect in the analyses performed. Therefore, LMI and MFR seem to be better mediators of muscle quantity in adolescents between the variable’s adiposity, cardiorespiratory and muscular fitness with the CRMF. To the best of our knowledge, this is one of the first studies to examine the mediating role of muscle mass quantity in the relationship between physical fitness and cardiometabolic risk score in adolescents.
The importance of our study is emphasized, since there is an inverse relationship between cardiometabolic risk and low muscle mass or disproportionate muscle mass (in relation to fat)15,16. The disproportionate between of fat and lean mass was mainly analyzed in the context of adults, the elderly, and/or those with chronic diseases15. In the elderly, this relationship is confirmed by the amount of ASM (kg) divided by the squared height (m−2), while for adults, the diagnosis is made by the ratio of ASM (kg) divided by BMI (kg/m−2), whose adjustment is intended to reduce the interference that weight may have on lean mass30. For youth, proposals for verifying muscle quality include the ratio of muscle mass and fat mass or MFR41, handgrip42,43 and LMI31. Thus, Ripka et al.31 conducted a study that established curves with percentiles for fat mass, lean mass, LMI, ASM by DXA for Brazilian adolescents. They proposed LMI values of the 3rd percentile as the lower limit, aiming to identify LM abnormalities in the 12- to 17-year-old age group, which can be used for the diagnosis of decreased lean mass and relate to cardiometabolic risk, especially in overweight adolescents. Thus, excess fat mass in relation to muscle mass may be associated with low muscle mass, by reduced strength (i.e. dyapenia), as well as reduced muscle function related to cardiometabolic factors, which usually accompany obesity.
In the present research, in the comparison between adiposity groups by BMI-z, we confirmed that body weight overload exerted daily muscle work in adolescents with obesity, demonstrated by higher LM and LMI, as well as higher RM-leg press compared to eutrophic and overweight adolescents. While the ASM and ASMI did not differ between the groups, denoting no discrimination of muscle quantity in adolescents. However, it is reinforced that we did not evidence the presence of disproportion between fat and lean mass in adolescents with obesity in the current study, whose LMI values were above the 3rd percentile31 and adolescents with obesity showed CRF similar to eutrophic adolescents, in which muscle quantity, represented by LMI and MFR, played a mediating role in the reduction of CMRF.
In other studies, adolescents with obesity also demonstrated greater absolute muscle strength compared to their non-obese peers, but showed low muscle strength relative to body mass, low muscle fitness, and reduced neuromuscular activation capacity14,16,44. Adolescents with obesity can compensate for their greater body weight by increasing the level of voluntary activation during muscle contraction45, which may reflect in positive adaptation of the neuromuscular system to weight-bearing tasks. However, adolescents with obesity exhibit higher energy expenditure in performing body movement and increased muscle fatigue rate during exercise, partially explaining their limited involvement in physical activities, reduced muscle fitness and mobility46. Therefore, they may have difficulty maintaining muscle strength due to being overweight and possibly cause muscle weakness, which in turn may be caused by reduced mobility, neural adaptations, and changes in muscle morphology.
In our study, in the analysis of the MFR we noticed that it was higher in eutrophic, whose indexes were followed in a decreasing manner by the overweight and then in the obese, because the advantage of the higher LM may present progressive impairment caused by the higher fat mass. However, adolescents with obesity showed no disadvantages in cardiorespiratory and muscular fitness, despite showing impairment in most of the mean cardiometabolic variables. Expected cardiometabolic outcomes, as overweight and obese children and adolescents are more likely to have early cardiometabolic risk factors, such as high blood pressure47, disorders in lipid metabolism47, in glucose metabolism48 and in the inflammatory process47. This can lead to the development of chronic diseases such as type 2 diabetes mellitus, non-alcoholic fatty liver disease, endothelial dysfunction, and musculoskeletal dysfunction in adulthood49,50.
Recent evidence has shown that dyapenia and muscle mass contribute to adverse cardiometabolic health outcomes in children and adolescents51. In Korean adolescents, low skeletal muscle mass was associated with metabolic syndrome, and even after controlling for confounding factors, the risk of metabolic syndrome was higher in adolescents with low muscle mass49. An observational study found that adolescents at the 25th percentile of muscle mass had higher waist circumference, blood pressure, triglycerides, TC/HDL-c, HOMA-IR, and metabolic syndrome z-score than their peers at other percentiles, as well as adolescents with low muscle mass and obesity had the most unfavorable cardiometabolic profile52.
Research suggests that a body composition phenotype, which combines high-fat mass and low muscle mass, may be associated with higher health risks in adults, compared to any one body composition compartment alone53,54. The underlying mechanisms by which obesity affects skeletal muscle remain poorly understood; however, lipid accumulation in skeletal muscle and chronic low-grade inflammation may contribute to muscle impairment44. The positive energy balance leads to excessive fat accumulation in the subcutaneous region and between skeletal muscle fibers55. Fat accumulation initiates a systemic inflammatory response characterized by infiltration of immune cells into skeletal muscle tissue and increased secretion and activation of pro-inflammatory cytokines by myocytes and adipocytes. Because of chronic exposure to pro-inflammatory cytokines, satellite cell function may be affected, as well as myoblast proliferation and differentiation, negatively impacting skeletal muscle maintenance and regeneration56.
In addition to muscle mass, muscle strength is also an important aspect of physical fitness14,44, a protective factor of physical and cardiometabolic health both in the adult and elderly population8 and in children and adolescents16,23. These studies suggest that both low muscle mass and low muscle strength are contributors to metabolic dysfunction in the pediatric population25, as well as early onset of hypertensive measures26. Recent evidence focuses on reduction in muscle mass and cardiometabolic changes16,23, as well as understanding the mediating role of muscle quantity in the relationship between adiposity and bone mineral content27. Furthermore, although the interaction between reduced muscle mass and associated morbidities have not been investigated in detail in children and adolescents, excess fat with low muscle mass probably arises in childhood, reducing mobility and agility in children and adolescents12, and consequently compromising motor competence in adolescents with obesity11 and metabolic health before adulthood57.
This study has some strengths and limitations. The strengths were to assess body composition by DXA, cardiorespiratory fitness by stress test with metabolic analyzer, and muscular fitness by the one repetition maximum test, considered the best methods for assessing physical fitness. We used some variables to compose a cardiometabolic risk score and were performed by valid and reliable methods for monitoring the adolescent’s health. Also, adolescence is a period of somatic and biological growth, and changes can confound the results, our analyses were controlled for sex, age, and somatic maturation (age at peak height velocity). Finally, as far as we know, this study may be the first to consider LMI as a mediator in the relationship between physical fitness and a relevant marker of cardiometabolic health. On the other hand, we consider the cross-sectional design as one of the limitations, for not allowing the inference of causality, as well as the sample size used does not allow the generalization of the results, factors that should be analyzed with caution.
The results found in this study provide data on the association of muscle quantity, physical fitness, and cardiometabolic risk in adolescents, factors that contribute to the prevention and maintenance of health in this population. We highlight that LMI was identified as a mediator of muscle quantity in the relationship between fat mass vs. CMRF in total adolescents, plus CRF vs. CMRF in girls, who generally have lower participation in regular physical activity. While in boys there was no significant relationship between adiposity, physical fitness and CRMF. In addition, the MFR showed a mediating role in the relationship between RM-leg press and CMRF. Therefore, we highlight the importance of muscle quantity as a mediator in physical fitness and fat mass, for the reduction of cardiometabolic risk factors, justifying the importance of a healthy lifestyle in children and adolescents, especially with emphasis on girls.








